Archived MIPS Program Requirements
View MIPS program requirements and measure workflows from previous performance years.
Traditional MIPS Performance Year 2024
Traditional MIPS requirements for the 2024 performance year are based on the Calendar Year 2024 Updates to the Physician Fee Schedule final rule.
For the 2024 performance year, the most significant change is the increased length of the Promoting Interoperability performance period from 90 days to 180 days. There were no changes to eligibility requirements, performance category weighting, or payment adjustments. The performance periods for the Quality, Cost, and Improvement Activities categories remain unchanged.
MIPS eligible clinicians are: Physicians, Osteopathic Practitioners, Chiropractors, Physician Assistants, Nurse Practitioners, Clinical Nurse Specialists, Certified Registered Nurse Anesthetists, Physical Therapists, Occupational Therapists, Clinical Psychologists, Qualified Speech-Language Pathologists, Qualified Audiologists, Registered Dietitian or Nutrition professionals, Clinical Social Workers, and Certified Nurse Midwives. Eligible clinicians must also exceed the Low-Volume Threshold as an individual or as part of a group.
In 2024, the Low-Volume Threshold applies to clinicians who:
-
Bill $90,000 or less in Medicare Part B allowed charges
Or
-
Provide care for 200 or fewer Medicare Part B patients
Or
- Provide 200 or fewer covered professional services to Medicare Part B patients
Still not sure if you qualify? Email the QPP Helpdesk at QPP@cms.hhs.gov. The QPP Participation Status Tool can also help you review your eligibility status throughout the year.
CMS measures EC performance through data submitted in four categories. These performance categories are weighted to comprise the MIPS composite score.
-
Quality: measures the quality of care delivered, based on measures related to healthcare quality and outcomes of patient care. Quality accounts for 30% of the MIPS composite score.
-
Cost: cost of care provided, calculated by CMS based on the EC’s Medicare administrative claims data. Cost accounts for 30% of the MIPS composite score.
-
Promoting Interoperability (PI): promotes the use of certified EHR technology for improved patient engagement and electronic exchange of information. PI accounts for 25% of the MIPS composite score.
-
Improvement Activities (IA): promotes innovation and ongoing improvement to clinical activities, with a focus on areas such as coordination of care, population management, and beneficiary engagement. IA accounts for 15% of the MIPS composite score.
The final MIPS composite score determines whether the EC will receive a positive, negative, or neutral payment adjustment. To avoid a negative payment adjustment, an EC must have a minimum score of 75 points (out of 100).
ECs can earn a positive payment adjustment on their Medicare Part B reimbursements based on MIPS performance in 2024. ECs who choose not to participate or who do not meet the minimum performance thresholds will receive a negative payment adjustment of up to -9%.
- Data for the Quality and Cost categories must be reported for the full calendar year.
- CMS uses Medicare administrative claims data to calculate Cost measure performance which means ECs do not have to submit any data for this performance category.
- Data for Promoting Interoperability must be reported for a minimum continuous 180-day period.
- Data for Improvement Activities must be reported for a minimum continuous 90-day period.
The submission period to report MIPS data for the 2024 performance year will begin January 1, 2025. The deadline to submit MIPS data for the 2024 performance year is March 31, 2025.
Traditional MIPS Performance Year 2023
Traditional MIPS requirements for the 2023 performance year are based on the Calendar Year 2023 Updates to the Physician Fee Schedule final rule.
For the 2023 performance year, the most significant change is the removal of the exceptional performance bonus. There were no changes to eligibility requirements, performance category weighting, payment adjustments, or performance period definition.
MIPS eligible clinicians are: Physicians, Physician Assistants, Nurse Practitioners, Osteopathic Practitioners, Chiropractors, Clinical Nurse Specialists, Certified Registered Nurse Anesthetists, Physical Therapists, Occupational Therapists, Qualified Speech-Language Pathologists, Qualified Audiologists, Clinical Psychologists, Registered Dietitian or Nutrition professionals, Clinical Social Workers, and Certified Nurse Midwives who exceed the Low-Volume Threshold.
In 2023, the Low-Volume Threshold applies to clinicians who:
-
Bill $90,000 or less in Medicare Part B allowed charges
Or
-
Provide care for 200 or fewer Medicare Part B patients
Or
- Provide 200 or fewer covered professional services to Medicare Part B patients
Still not sure if you qualify? Email the QPP Helpdesk at QPP@cms.hhs.gov. The QPP Participation Status tool can also help you review your eligibility status throughout the year.
CMS measures EC performance through data submitted in four categories. These performance categories are weighted to comprise the MIPS composite score.
Quality: measures the quality of care delivered, based on measures related to healthcare quality and outcomes of patient care. Quality accounts for 30% of the MIPS composite score.
Cost: cost of care provided, calculated by CMS based on the EC’s Medicare claims data. Cost accounts for 30% of the MIPS composite score.
Promoting Interoperability (PI): promotes the use of certified EHR technology for improved patient engagement and electronic exchange of information. PI accounts for 25% of the MIPS composite score.
Improvement Activities (IA): promotes innovation and ongoing improvement to clinical activities, with a focus on areas such as coordination of care, population management, and beneficiary engagement. IA accounts for 15% of the MIPS composite score.
The final MIPS composite score determines whether the EC will receive a positive, negative, or a neutral payment adjustment. To avoid a negative payment adjustment, an EC must have a minimum score of 75 points (out of 100).
ECs can earn a positive payment adjustment on their Medicare Part B reimbursements based on MIPS performance in 2023. ECs who choose not to participate or who do not meet the minimum performance thresholds will receive a negative payment adjustment of up to -9%.
- Data for the Quality and Cost categories must be reported for the full calendar year.
- CMS uses Medicare Part A and B claims data to calculate Cost measure performance which means ECs do not have to submit any data for this performance category.
- Data for Promoting Interoperability and Improvement Activities must be reported for a minimum continuous 90-day period.
The submission period to report MIPS data for the 2023 performance year will begin in January 2, 2024. The deadline to submit MIPS data for the 2023 performance year is April 15, 2024.
Traditional MIPS Performance Year 2022
Traditional MIPS requirements for the 2022 performance year are based on the Calendar Year 2022 Updates to the Quality Payment Program final rule.
The requirements for MIPS participation change based on the scheduled implementation of the program as established by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and by annual rule-making published by CMS.
For the 2022 performance year, the most significant changes are the re-weighting of the Quality category to 30% and the Cost category to 30% of the total MIPS score and the addition of two new eligible clinician types: Clinical social workers and Certified nurse mid-wives. The performance threshold has also increased to 75 points, an increase of 15 points from the previous year. Notably, there are no changes to low-volume threshold levels for eligibility, payment adjustments, or performance period definition.
MIPS eligible clinicians are: Physicians, Physician Assistants, Nurse Practitioners, Osteopathic Practitioners, Chiropractors, Clinical Nurse Specialists, Certified Registered Nurse Anesthetists, Physical Therapists, Occupational Therapists, Qualified Speech-Language Pathologists, Qualified Audiologists, Clinical Psychologists, Registered Dietitian or Nutrition professionals, Clinical Social Workers, and Certified Nurse Mid-wives who exceed the Low-Volume Threshold.
In 2022, the Low-Volume Threshold applies to clinicians who:
-
Bill $90,000 or less in Medicare Part B allowed charges
Or
-
Provide care for 200 or fewer Part B-enrolled individuals
Or
- Provide 200 or fewer covered professional services to Part B-enrolled individuals
Still not sure if you qualify? Email the QPP Helpdesk at QPP@cms.hhs.gov. The QPP Participation Status tool can also help you review your eligibility status throughout the year.
CMS measures EC performance through data submitted in four categories. These performance categories are weighted to comprise the MIPS composite score.
-
Quality: measures the quality of care delivered, based on measures related to healthcare quality and outcomes of patient care. Quality accounts for 30% of the MIPS composite score.
-
Cost: cost of care provided, calculated by CMS based on the EC’s Medicare claims data. Cost accounts for 30% of the MIPS composite score.
-
Promoting Interoperability (PI): promotes the use of certified EHR technology for improved patient engagement and electronic exchange of information. PI accounts for 25% of the MIPS composite score.
-
Improvement Activities (IA): promotes innovation and ongoing improvement to clinical activities, with a focus on areas such as coordination of care, population management, and beneficiary engagement. IA accounts for 15% of the MIPS composite score.
The final MIPS composite score determines whether the EC will receive a positive, negative, or neutral payment adjustment. To avoid a negative payment adjustment, an EC must have a minimum score of 75 points (out of 100).
ECs can earn a positive payment adjustment of up to +9% on their Medicare Part B reimbursements based on MIPS performance in 2022. ECs who choose not to participate or who do not meet the minimum performance thresholds will receive a negative payment adjustment of up to -9%. ECs with performance scores of 89 points and higher are eligible for an exceptional performance bonus.
- Data for the Quality and Cost categories must be reported for the full calendar year.
- CMS uses Medicare Part A and B claims data to calculate Cost measure performance which means ECs do not have to submit any data for this performance category.
- Data for Promoting Interoperability and Improvement Activities must be reported for a minimum continuous 90-day period.
The submission period to report MIPS data for the 2022 performance year will begin on January 4, 2023.
The deadline to submit MIPS data for the 2022 performance year is March 31, 2023.
MIPS Performance Year 2021
MIPS requirements for the 2021 performance year are based on the Calendar Year 2021 Updates to the Quality Payment Program final rule.
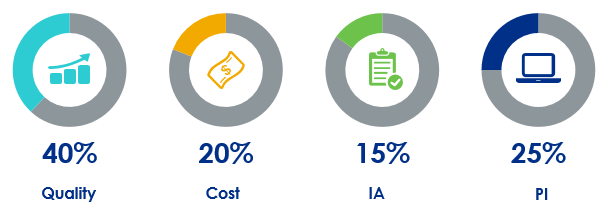
The requirements for MIPS participation change based on the scheduled implementation of the program as established by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and by annual rule-making published by CMS. For the 2021 performance year, the most significant changes for ECs are to the re-weighting of the Quality category to 40% and the Cost category to 20% of the total MIPS score. The performance threshold has also increased to 60 points. Notably, there are no changes to MIPS eligible clinician types, low volume threshold levels, payment adjustments, or performance period definition.
MIPS eligible clinicians are: Physicians, Physician Assistants, Nurse Practitioners, Clinical Nurse Specialists, Certified Registered Nurse Anesthetists, Physical Therapists, Occupational Therapists, Qualified Speech-Language Pathologists, Qualified Audiologists, Clinical Psychologists, and Registered Dietitian or Nutrition professionals who exceed the Low-Volume Threshold.
In 2021, the Low-Volume Threshold applies to clinicians who:
-
Bill $90,000 or less in Medicare Part B allowed charges
Or
-
Provide care for 200 or fewer Part B-enrolled individuals
Or
- Provide 200 or fewer covered professional services to Part B-enrolled individuals
Still not sure if you qualify? Email the QPP Helpdesk at QPP@cms.hhs.gov. The QPP Participation Status tool can also help you review your eligibility status throughout the year.
CMS measures EC performance through data submitted in four categories. These performance categories are weighted to comprise the MIPS composite score.
Quality: measures the quality of care delivered, based on measures related to healthcare quality and outcomes of patient care. Quality accounts for 40% of the MIPS composite score.
Cost: cost of care provided, calculated by CMS based on the EC’s Medicare claims data. Cost accounts for 20% of the MIPS composite score.
Promoting Interoperability (PI): promotes the use of certified EHR technology for improved patient engagement and electronic exchange of information. PI accounts for 25% of the MIPS composite score.
Improvement Activities (IA): promotes innovation and ongoing improvement to clinical activities, with a focus on areas such as coordination of care, population management, and beneficiary engagement. IA accounts for 15% of the MIPS composite score.
The final MIPS composite score determines whether the EC will receive a positive, negative, or a neutral payment adjustment. To avoid a negative payment adjustment, an EC must have a minimum score of 60 points (out of 100).
ECs can earn a positive payment adjustment of up to +9% on their Medicare Part B reimbursements based on MIPS performance in 2021. ECs who choose not to participate or do not meet the minimum performance thresholds will receive a negative payment adjustment of up to -9%. Positive and negative payment adjustments are scheduled to increase each year of the program, with performance bonuses awarded to the highest scoring ECs.
- Data for the Quality and Cost categories must be reported for the full calendar year.
- CMS uses Medicare Part A and B claims data to calculate Cost measure performance which means ECs do not have to submit any data for this performance category.
- Data for Promoting Interoperability and Improvement Activities must be reported for a minimum continuous 90-day period.
The submission period to report MIPS data for the 2021 performance year will begin on January 3, 2022.
The deadline to submit MIPS data for the 2021 performance year is March 31, 2022.
MIPS Performance Year 2020
The requirements for MIPS participation change based on the scheduled implementation of the program as established by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and by annual rule-making published by CMS. There are less significant changes for the 2020 performance year (MIPS Year 4) compared to years past to allow ECs to focus on improved performance across all performance categories. Notably, there are no changes to MIPS eligible clinician types, low volume threshold levels, performance category scoring methodologies, performance period definition, or CEHRT![]() Certified EHR Technology, an EHR that conforms to the ONC's Health IT Certification Program criteria and standards requirements.
Certified EHR Technology, an EHR that conforms to the ONC's Health IT Certification Program criteria and standards requirements.
MIPS eligible clinicians are: Physicians, Physician Assistants, Nurse Practitioners, Clinical Nurse Specialists, Certified Registered Nurse Anesthetists, Physical Therapists, Occupational Therapists, Qualified Speech-Language Pathologists, Qualified Audiologists, Clinical Psychologists, and Registered Dietitian or Nutrition professionals who exceed the Low-Volume Threshold.
In 2020, the Low-Volume Threshold applies to clinicians who:
-
Bill $90,000 or less in Medicare Part B allowed charges
Or
-
Provide care for 200 or fewer Part B-enrolled individuals
Or
- Provide 200 or fewer covered professional services to Part B-enrolled individuals
Still not sure if you qualify? Email the QPP Helpdesk at QPP@cms.hhs.gov. The QPP Participation Status tool can also help you review your eligibility status throughout the year.
CMS measures EC performance through data submitted in four categories. These performance categories are weighted to comprise the MIPS composite score.
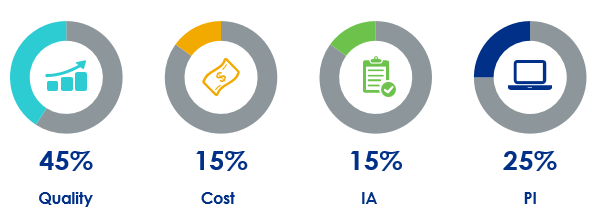
Quality: measures the quality of care delivered, based on measures related to healthcare quality and outcomes of patient care. Quality accounts for 45% of the MIPS composite score.
Cost: cost of care provided, calculated by CMS based on the EC’s Medicare claims data. Cost accounts for 15% of the MIPS composite score.
Promoting Interoperability (PI): promotes the use of certified EHR technology for improved patient engagement and electronic exchange of information. PI accounts for 25% of the MIPS composite score.
Improvement Activities (IA): promotes innovation and ongoing improvement to clinical activities, with a focus on areas such as coordination of care, population management, and beneficiary engagement. IA accounts for 15% of the MIPS composite score.
The final MIPS composite score determines whether the EC will receive a positive, negative, or a neutral payment adjustment. To avoid a negative payment adjustment, an EC must have a minimum score of 45 points (out of 100).
ECs can earn a positive payment adjustment of up to +9% on their Medicare Part B reimbursements based on MIPS performance in 2020. ECs who choose not to participate or do not meet the minimum performance thresholds will receive a negative payment adjustment of up to -9%. Positive and negative payment adjustments are scheduled to increase each year of the program, with performance bonuses awarded to the highest scoring ECs.
- Data for the Quality and Cost categories must be reported for the full calendar year.
- CMS uses Medicare Part A and B claims data to calculate Cost measure performance which means ECs do not have to submit any data for this performance category.
- Data for Promoting Interoperability and Improvement Activities must be reported for a minimum continuous 90-day period.
The submission window to report MIPS data for the 2020 performance year begins on January 4, 2021.
The deadline to submit MIPS data for the 2020 performance year is March 31, 2021.
MIPS Performance Year 2019
MIPS Year 3 is the set of program rules and requirements for the 2019 performance year. The requirements for MIPS participation change based on the scheduled implementation of the program as established by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and by annual rule-making published by CMS.
Requirements for MIPS in performance year 3 are based on the Calendar Year 2019 Updates to the Quality Payment Program final rule.
MIPS eligible clinicians are: Physicians, Physician Assistants, Nurse Practitioners, Clinical Nurse Specialists, Certified Registered Nurse Anesthetists, Physical Therapists, Occupational Therapists, Qualified Speech-Language Pathologists, Qualified Audiologists, Clinical Psychologists, and Registered Dietitian or Nutrition professionals who exceed the Low-Volume Threshold.
For MIPS Year 3, the Low-Volume Threshold applies to clinicians who:
-
Bill $90,000 or less in Medicare Part B allowed charges
Or
-
Provide care for 200 or fewer Part B-enrolled individuals
Or
- Provide 200 or fewer covered professional services to Part B-enrolled individuals
Still not sure if you qualify? Email the QPP Helpdesk at QPP@cms.hhs.gov. The QPP Participation Status tool can also help you review your eligibility status throughout the year.
CMS measures EC performance through data submitted in four categories. These performance categories are weighted to comprise the MIPS composite score.
Quality: measures the quality of care delivered, based on measures related to healthcare quality and outcomes of patient care. Quality accounts for 45% of the MIPS composite score.
Cost: cost of care provided, calculated by CMS based on the EC’s Medicare claims data. Cost accounts for 15% of the MIPS composite score.
Promoting Interoperability (PI): promotes the use of certified EHR technology for improved patient engagement and electronic exchange of information. PI accounts for 25% of the MIPS composite score.
Improvement Activities (IA): promotes innovation and ongoing improvement to clinical activities, with a focus on areas such as coordination of care, population management, and beneficiary engagement. IA accounts for 15% of the MIPS composite score.
The final MIPS composite score determines whether the EC will receive a positive, negative, or a neutral payment adjustment. To avoid a negative payment adjustment, an EC must have a minimum score of 30 points (out of 100).
ECs can earn a positive payment adjustment of up to a 7% on their Medicare Part B reimbursements based on MIPS performance in 2019. ECs who choose not to participate or do not meet the minimum performance thresholds will receive a -7% payment adjustment. Positive and negative payment adjustments are scheduled to increase each year of the program, with performance bonuses awarded to the highest scoring ECs.
Data for the Quality and Cost categories must be reported for the full calendar year. Data for Promoting Interoperability and Improvement Activities can be reported for a minimum continuous 90-day period or for the full calendar year.
The submission window to report MIPS data for the 2019 performance year begins on January 2, 2020.
The deadline to submit MIPS data for the 2019 performance year is April 30, 2020.
MIPS Performance Year 2018
MIPS Year 2 is the set of program rules and requirements for the 2018 performance year. There were significant changes from MIPS Year 1 to MIPS Year 2, and more changes can be expected for MIPS Year 3 (2019).
Requirements for MIPS in performance year 2 are based on the Calendar Year 2018 Updates to the Quality Payment Program final rule.
MIPS eligible clinicians are Physicians, Physician Assistants, Nurse Practitioners, Clinical Nurse Specialists, and Certified Registered Nurse Anesthetists who:
-
Bill more than $90,000 in Medicare Part B services per year
Or
- Provide care for more than 200 Medicare Part B patients per year
Still not sure if you qualify? Use the QPP Participation Status tool to review your eligibility status throughout the year.
CMS measures EC performance through data submitted for four reporting categories:
- Quality: measures the quality of care delivered, based on measures related to healthcare quality and outcomes of patient care. Quality accounts for 50% of the MIPS composite score.
- Cost: cost of care provided, calculated by CMS based on the EC’s Medicare claim data. Cost accounts for 10% of the MIPS composite score.
- Promoting Interoperability (PI): promotes the use of certified EHR technology for improved patient engagement and electronic exchange of information. PI accounts for 25% of the MIPS composite score.
- Improvement Activities (IA): promotes innovation and ongoing improvement to clinical activities, with a focus on areas such as coordination of care, population management, and beneficiary engagement. IA accounts for 15% of the MIPS composite score.
The final MIPS composite score determines whether the EC will receive a positive, negative, or a neutral payment adjustment. To avoid a negative payment adjustment, an EC must have a minimum score of 15 points (out of 100).
ECs can earn a positive payment adjustment of up to a 5% on their Medicare Part B reimbursements based on MIPS performance in 2018. ECs who choose not to participate or do not meet the minimum performance thresholds will receive a -5% payment adjustment. Positive and negative payment adjustments are scheduled to increase each year of the program, with performance bonuses awarded to the highest scoring ECs.
Data for the Quality and Cost categories must be reported for the full calendar year. Data for Promoting Interoperability and Improvement Activities can be reported for a minimum continuous 90-day period or for the full calendar year.
The submission window to report MIPS data for the 2018 performance year begins on January 2, 2019 at 10:00am ET
The deadline to submit MIPS data for the 2018 performance year is April 2, 2019 at 8:00pm ET
Note: If submitting MIPS data via Claims, the submission deadline is March 2, 2019.
Didn't find the answer you were looking for?
Contact Sevocity Support 24/7 at 877‑777‑2298 or support@sevocity.com