CMS 159v11: Depression Remission at Twelve Months
| Measure: The percentage of adolescent patients 12 to 17 years of age and adult patients 18 years of age or older with major depression or dysthymia who reached remission 12 months (+/- 60 days) after an index event | ||
| Measure Type | High Priority Measure | Scoring |
| Outcome | Yes | A higher percentage indicates better quality |
| Denominator | Adolescent patients 12 to 17 years of age and adult patients 18 years of age and older with a diagnosis of major depression or dysthymia and an initial PHQ-9 or PHQ-9M score greater than nine during the index event. Patients may be assessed using PHQ-9 or PHQ-9M on the same date or up to 7 days prior to the encounter (index event) |
| Numerator | Adolescent patients 12 to 17 years of age and adult patients 18 years of age and older who achieved remission at twelve months as demonstrated by the most recent twelve month (+/- 60 days) PHQ-9 or PHQ-9M score of less than five |
| Denominator Exceptions | None |
| Denominator Exclusions |
|
Patients who meet the following criteria will be included in the denominator:
-
Age is ≥ 12 years at the time of the initial PHQ-9 assessment
AND
-
Have a PHQ-9 score > 9 on the day of the eligible encounter or in the 7 days prior to the encounter
AND
- Have at least one eligible encounter with an active diagnosis of major depression or dysthymia in the 14 to 2 months prior to the Measurement Period finalized by the EC
CPT: 90791, 90972, 90832, 90833, 90834, 90836, 90837, 90838, 90839, 90840, 96156, 96158, 96159, 99202, 99203, 99204, 99205, 99211, 99212, 99213, 99214, 99215, 99384, 99385, 99386, 99387, 99394, 99395, 99396, 99397, 99421, 99422, 99423, 99441, 99442, 99443
HCPCS: G0402, G0438, G0439
Diagnoses are documented in the Assessment tab of an encounter. The eligible diagnosis codes for major depression and dysthymia are:
Major Depression
ICD-10: F32.0, F32.1, F32.2, F32.3, F32.4, F32.5, F32.9 , F33.0, F33.1, F33.2 , F33.3, F33.40, F33.41 , F33.42, F33.9
Dysthymia
ICD-10: F34.1
To document a PHQ-9 assessment:
- Go to Encounter > Flowsheets/Labs > Standard or Chart > Flowsheets/Labs > Standard
- Click Add New Flowsheet
- Select the PHQ-9 flowsheet and click Add
- Click Add Column
- Select a Value for all questions in the PHQ-9
- Click OK to save
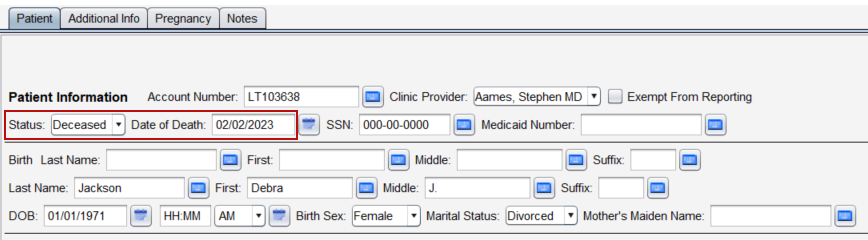
A patient will be excluded from the measure if they meet any of the following conditions:
-
Died any time prior to the end of the measure assessment period
-
Received hospice or palliative care services between the start of the denominator period and the end of the measurement assessment period
-
Was a permanent nursing home resident between the start of the denominator period and the end of the measurement assessment period
-
Had a diagnosis of bipolar disorder, personality disorder emotionally labile, schizophrenia or psychotic disorder, or pervasive developmental disorder any time prior to the end of the measure assessment period
To document hospice care ambulatory services, go to Encounter > Orders/Procedure > Orders/Referrals and click Add to add one of the eligible codes listed below:
CPT: 99377, 99378
HCPCS: G0182
Order Status must be marked as Pending or Complete.
To document hospice care encounter services, go to Encounter > Orders/Procedure > Orders/Referrals and click Add to add one of the eligible codes listed below:
HCPCS: G9996, G9473, G9474, G9475, G9476, G9477, G9478, G9479, Q5003, Q5004, Q5005, Q5006, Q5007, Q5008, Q5010, S9126, T2042, T2043, T2044, T2045, T2046
Order Status must be marked as Complete.
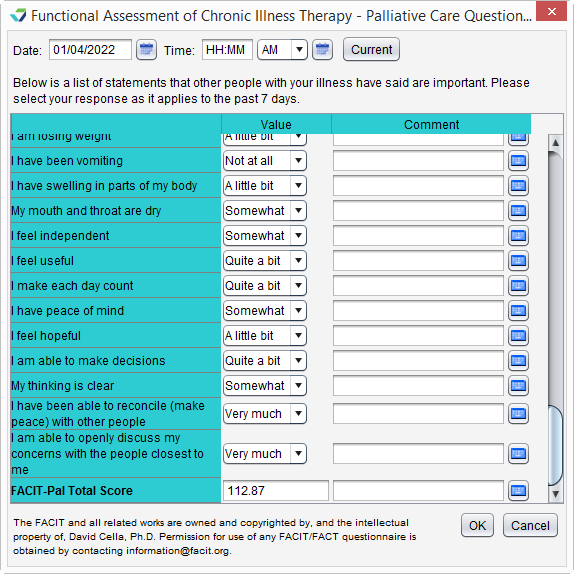
Palliative care services can be documented using the FACIT-Pal Questionnaire flowsheet, as an order, or as a diagnosis.
Go to Encounter > Orders/Procedure > Orders/Referrals and click Add to add one of the eligible codes listed below:
HCPCS: G9054, M1017
Order Status must be marked as Complete.
Diagnoses are documented in the Assessment tab of an encounter. The eligible diagnosis code for palliative care is:
ICD-10: Z51.5
To document nursing home stay using the Admissions tab:
-
Go to Chart > Admissions and click Add
-
Select Long Term Care as Place of Service
-
Optional: select a Facility
-
Populate the Admit Date
-
Optional: populate the Discharge Date
-
Note: if populated, the Discharge Date must be after the end of the measure assessment period to qualify as a patient exclusion
-
-
Click OK
To document nursing home stay using the Orders tab, go to Encounter > Orders/Procedure > Orders/Referrals and click Add to add one of the eligible codes listed below:
CPT: 99324, 99325, 99326, 99327, 99328, 99334, 99335, 99336, 99337
Order Status must be marked as Complete.
A patient will be counted in the numerator if they achieved depression remission at twelve months as demonstrated by the most recent twelve month (+/- 60 days) PHQ-9 score less than five.
To document a PHQ-9 assessment:
- Go to Encounter > Flowsheets/Labs > Standard or Chart > Flowsheets/Labs > Standard
- Click Add New Flowsheet
- Select the PHQ-9 flowsheet and click Add
- Click Add Column
- Select a Value for all questions in the PHQ-9
- Click OK to save
Return to 2023 eCQMs
Didn't find the answer you were looking for?
Contact Sevocity Support 24/7 at 877‑777‑2298 or support@sevocity.com