CMS 165v10: Controlling High Blood Pressure
| Measure: Percentage of patients 18-85 years of age who had a diagnosis of essential hypertension starting before and continuing into, or starting during the first six months of the measurement period, and whose most recent blood pressure was adequately controlled (<140/90mmHg) during the measurement period | ||
| Measure Type | High Priority Measure | Scoring |
| Outcome | Yes | A higher percentage indicates better quality |
| Denominator | Patients 18-85 years of age who had a visit and diagnosis of essential hypertension starting before and continuing into, or starting during the first six months of the measurement period |
| Numerator | Patients whose most recent blood pressure is adequately controlled (systolic blood pressure < 140 mmHg and diastolic blood pressure < 90 mmHg) during the measurement period |
| Denominator Exceptions | None |
| Denominator Exclusions |
|
Patients who meet the following criteria will be included in the denominator:
-
Age is ≥ 18 years and < 85 years at the beginning of the Measurement Period
AND
-
Have an active diagnosis of essential hypertension at the start of the Measurement Period or were diagnosed with essential hypertension within the first six months of the Measurement Period
AND
- Must have at least one eligible encounter during the Measurement Period finalized by the EC
CPT: 99201, 99202, 99203, 99204, 99205, 99212, 99213, 99214, 99215, 99395, 99396, 99397, 99385, 99386, 99387, 99341, 99342, 99343, 99344, 99345, 99347, 99348, 99349, 99350, 98969, 98970, 98971, 98972, 99421, 99422, 99423, 99458, 98966, 98967, 98968, 99441, 99442, 99443
HCPCS: G0438, G0439, G0071, G2010, G2012, G2061, G2062, G2063
The patient must have an active diagnosis of essential hypertension at the start of the Measurement Period or be diagnosed with essential hypertension within the first six months of the Measurement Period. Diagnoses are documented in the Assessment tab of an encounter.
The eligible diagnosis codes for essential hypertension are:
ICD-10: I10
ICD-9: 401.0, 401.1, 401.9
A patient will be excluded from this measure if they meet any of the following conditions:
- Has an active diagnosis of pregnancy, end stage renal disease, kidney transplant recipient, or chronic kidney disease, stage 5 during the Measurement Period
- Received services related to kidney disease or a kidney transplant before or during the Measurement Period
- Is in hospice care for any part of the Measurement Period
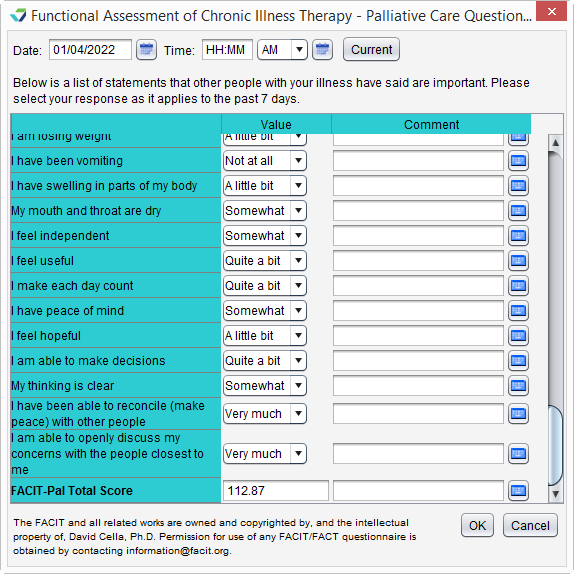
- Is receiving palliative care during the Measurement Period
- Age is ≥ 65 at the start of the Measurement Period and has spent more than 90 consecutive days during the Measurement Period living in long term care
- Age is ≥ 65 at the start of the Measurement Period and has evidence of frailty and advanced illness
- Age is ≥ 81 at the start of the Measurement Period and has evidence of frailty for any part of the Measurement Period
Diagnoses are documented in the Assessment tab of an encounter. A comprehensive list of eligible diagnosis codes for this exclusion can be located here.
To document the performance of a services received related to kidney disease or a kidney transplant, go to Encounter > Orders/Procedure > Orders/Referrals and click Add to add one of the eligible codes listed below. Order Status must be marked as Complete in order to count as an exclusion.
Dialysis Services
CPT: 90947, 90945, 90940, 90937, 90935
HCPCS: G0257
Kidney Transplant
CPT: 50300, 50320, 50340, 50380, 50370, 50365, 50360
HCPCS: S2065
ESRD Monthly Outpatient Services
CPT: 90951, 90952, 90953, 90954, 90955, 90956, 90957, 90958, 90959, 90960, 90961, 90962, 90963, 90964, 90965, 90966, 90967, 90968, 90969, 90970, 90989, 90993, 90997, 90999, 99512
To document hospice care services as a procedure, go to Encounter > Orders/Procedure > Orders/Referrals and click Add to add one of the eligible codes listed below:
SNOMED CT: 385763009, 385765002
Order Status must be marked as Pending or Complete.
SNOMED CT codes must be added as a Favorite in Preferences > Form Data > Orders to be accessible from the Orders/Referrals tab.
Palliative care services can be documented using the FACIT-Pal Questionnaire flowsheet or in the Orders/Procedure tab.
Go to Encounter > Orders/Procedure > Orders/Referrals and click Add to add one of the eligible codes listed below:
HCPCS: G9054, M1017
Order Status must be marked as Complete.
To document a stay in long term care:
- Go to Chart > Admissions and click Add
- Select a Place of Service
- Optional: select a Facility
- Populate the Admit Date
- Optional: populate the Discharge Date
- Click OK
If the admissions event does not have a Discharge Date when the eCQM report is generated, the length of stay will be calculated with a discharge date of the Reporting Period end date or the Measurement Period end date, whichever occurs first.
A patient has evidence of frailty if they meet any of the following criteria:
- Has an active diagnosis of Frailty during the Measurement Period
- Has an active diagnosis of Frailty Symptom during the Measurement Period
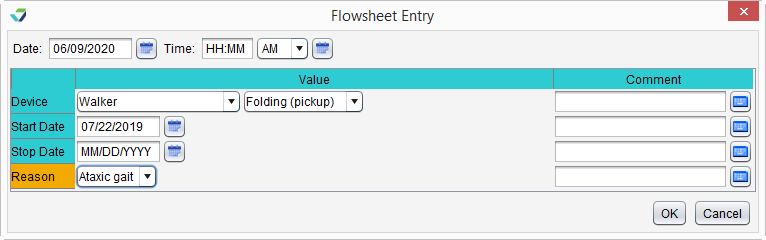
- Is using a frailty device during the Measurement Period
- Has a frailty encounter during the Measurement Period
"Frailty" refers to a range of conditions that includes falls and problems affecting mobility.
Diagnoses are documented in the Assessment tab of an encounter. A comprehensive list of eligible diagnosis codes for frailty can be located here.
Diagnoses are documented in the Assessment tab of an encounter. The eligible diagnosis codes for frailty symptoms are:
ICD-10: R26.0, R26.1, R26.2, R26.89, R26.9, R41.81, R53.1, R53.81, R53.83, R54, R62.7, R63.4, R63.6, R64
To document the patient's use of a frailty device:
- Go to Encounter > Flowsheets/Labs > Standard Flowsheets
- Click Add New Flowsheet
- Select the Frailty Device flowsheet and click Add
- Click Add Column
- Select a Device and the type (Value) of device
- Populate a usage Start Date for the device
- Optional: populate a usage Stop Date for the device
- The Stop Date cannot occur prior to the start of the Measurement Period
- Optional: populate a Reason for use of the device
- Click OK to save
CPT: 99504, 99509
HCPCS: G0162, G0299, G0300, G0493, G0494, S0271, S0311, S9123, S9124, T1000, T1001, T1002, T1003, T1004, T1005, T1019, T1020, T1021, T1022, T1030, T1031
A patient has evidence of advanced illness if they meet any of the following criteria:
- Had an inpatient encounter with an active diagnosis of Advanced Illness during the Measurement Period or in the year prior
- Had 2 or more outpatient encounters with an active diagnosis of Advanced Illness during the Measurement Period or in the year prior
- Encounters must have different dates of service
- Diagnosis must be active during all eligible encounters
- Was prescribed medication for dementia during the Measurement Period or in the year prior
"Advanced illness" refers to a wide range of conditions and includes diseases such as Alzheimer's disease, cancer, and heart failure.
Diagnoses are documented in the Assessment tab of an encounter. A comprehensive list of eligible diagnosis codes for advanced illness can be located here.
CPT: 99221, 99222, 99223, 99231, 99232, 99233, 99238, 99239, 99251, 99252, 99253, 99254, 99255, 99291
CPT: 99201, 99202, 99203, 99204, 99205, 99211, 99212, 99213, 99214, 99215, 99241, 99242, 99243, 99244, 99245, 99341, 99342, 99343, 99344, 99345, 99347, 99348, 99349, 99350, 99381, 99382, 99383, 99384, 99385, 99386, 99387, 99391, 99392, 99393, 99394, 99395, 99396, 99397, 99401, 99402, 99403, 99404, 99411, 99412, 99429, 99455, 99456, 99483, 99217, 99218, 99219, 99220, 99281, 99282, 99283, 99284, 99285, 99304, 99305, 99306, 99307, 99308, 99309, 99310, 99315, 99316, 99318, 99324, 99325, 99326, 99327, 99328, 99334, 99335, 99336, 99337
HCPCS: G0402, G0438, G0439, G0463, T1015
To prescribe a medication, go to Encounter > Medications > Manage/Prescribe Meds > New Prescription. A comprehensive list of eligible dementia medications can be located here.
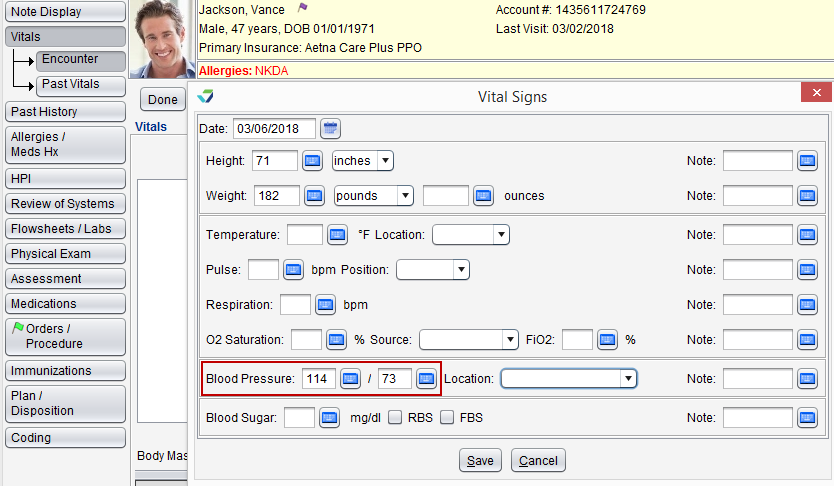
A patient will be counted in the numerator if they have a documented blood pressure reading of < 140/90 during their most recent encounter during the Measurement Period.
- Blood pressure readings taken during an emergency department visit will not count toward the numerator
- If no blood pressure is recorded during the Measurement Period, the patient’s blood pressure is assumed not controlled
- If there are multiple blood pressure readings on the same day, the lowest systolic and the lowest diastolic reading will be counted toward the numerator
Return to 2022 eCQMs
Didn't find the answer you were looking for?
Contact Sevocity Support 24/7 at 877‑777‑2298 or support@sevocity.com